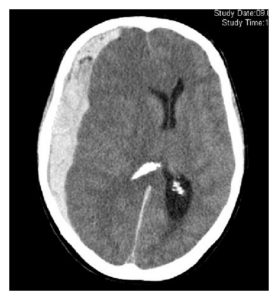
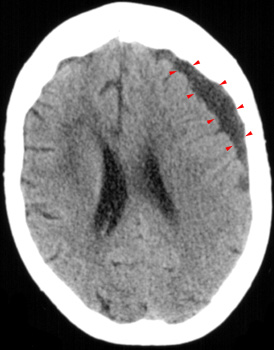
Subdural hematoma is a blood collection between the dura mater and the arachnoid that may be present in ~10% of head traumas. It is visible as a crescent-shaped lesion on the CT scan. Subdural hematomas may be classified as acute (one to two days), subacute (3-14 days) or chronic (>15 days).
CAUSES:
Subdural hematomas occur mostly due to traumatic rupture of bridging veins that drain the surface of the brain. The bleeding may stop spontaneously due to increased intracranial pressure or clot formation and that`s why subdural hematomas are often diagnosed only after several days or weeks.
On children, an important cause is inflicted head injury (shaken baby syndrome).
Other causes that are not as common include arterial injury, AV malformation, tumor or metastasis bleeding, aneurysm rupture or neurosurgical complication.
SIGNS & SYMPTOMS:
Symptoms may occur right after the trauma or latter in the course.
There is a wide variety of possible neurological symptoms, from headache to deep confusion and coma. In acute subdural hematomas, coma may be present in half of the patients, while the other half can present with different degrees of altered mental status or even asymptomatic at the beginning.
Signs and symptoms of elevated intracranial pressure may be present (headache, vomiting, bradycardia, hypertension, cranial nerve palsies, among others).
Chronic subdural hematoma may have insidious symptoms (headache, apathy, cognitive decline, lightheadedness, somnolence, seizures) and it can be hard to diagnose on elderly patients.
DIAGNOSIS:
A history of trauma is usually present. A comprehensive physical and neurological examination should be performed.
Imaging of the head is what confirm the diagnosis. On the CT scan, an acute hematoma appear as a hyperdense crescent-shaped lesion, whereas chronic hematomas are hypodense. MRI is more sensitive than CT scan, particularly for small hematomas.
Angiography (CTA or MRA) may be useful to identify the source of bleeding.
Prognostic indicators include age, neurological status (GCS), hematoma thickness, volume, presence and degree of midline shift, and reduced patency of the basal cisterns.
TREATMENT:
Acute hematomas are an emergency that should be treated promptly. After stabilization of the traumatized patient (ABC) a CT scan should be obtained.
Most acute cases will need surgical evacuation. Few selected patients (patients that are not deteriorating – with or without coma, with clot thickness <10mm, midline shift <5mm, no pupillary abnormalities and no elevated ICP) may received conservative treatment with ICU monitoring, serial CT scans and intracranial pressure monitoring.
Patients with chronic hematomas and evidence of cognitive impairment or progressive deterioration may also benefit from surgical evacuation.
If the patient was being anticoagulated, the anticoagulation should be reversed (cessation of the drug, vitamin K 10mg IV slowly, infusion of Prothrombin Complex Concentrate or fresh frozen plasma – all to reach an INR <1.2).
SOURCES & FURTHER READING:
- Brain Trauma Foundation. Severe TBI Guidelines. ©2010 Brain Trauma Foundation.
- Kentaro M, Maeda M. Surgical Treatment of Chronic Subdural Hematoma in 500 Consecutive Cases: Clinical Characteristics, Surgical Outcome, Complications, and Recurrence Rate. Neurol Med Chir (Tokyo) 41, 371-381, 2001.
- Alves JL et al. A Standardized Classification for Subdural Hematomas. Am J Forensic Med Pathol Volume 00, Number 00, Month 2016.
- Frontera JA et al. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage. Neurocrit Care. 2015.