Screening for three conditions is particularly important for female patients: Cervical cancer, Osteoporosis and Breast Cancer. Below we will review the guidelines regarding the screening for these conditions. Keep in mind that the recommendations may have variations depending on different instutitions` guidelines.
CERVICAL CANCER SCREENING GUIDELINES:
Who to screen?
Woman between 21 and 65 (over 65 only in certain situations, described below)
How to screen:
21-29 – Pap Smear
30-65 – Pap Smear + HPV testing (preferred method) OR Pap smear (acceptable)
How often to screen:
21-29 – Every 3 years (Pap Smear)
30-65 – Every 5 years (Pap Smear + HPV testing) OR Every 3 years (Pap Smear)
When to stop screening:
Aged >65 years with adequate negative prior screening* results and no history of CIN 2 or higher.
* Adequate prior screening = 3 consecutive negative cytology results OR 2 consecutive negative HPV results within 10 years before cessation of screening, with the most recent test occurring within 5 years.
When to continue screening after 65:
Women > 65 with inadequate prior screening OR history of CIN2 or higher should continue routine screening (Pap Smear every 3 years or Pap Smear + HPV cotesting every 5 years) for at least 20 years after spontaneous regression or appropriate management of the high-grade lesion.
Important points:
HPV testing alone is not recommended for any age group.
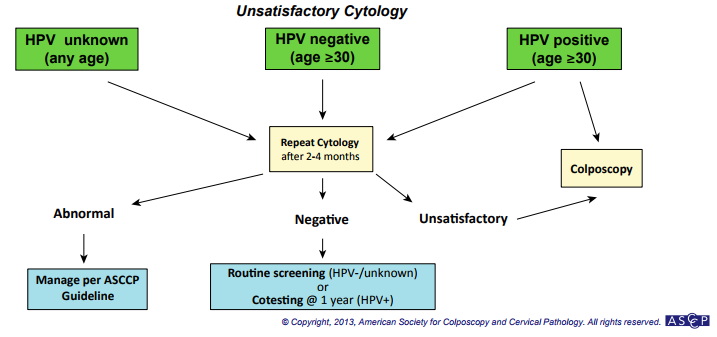
Unsatisfactory cytology should be repeated in 2-4 months.
If there is no cervix, there is no need for cervical cancer screening !
Some patients may benefit from more frequent screening (HIV, immunocompromise, history of high-grade dysplasia, in utero exposure to diethylstilbestrol). HIV patients, for instance, may benefit from screening at time of diagnoses and every 6 months for the first year. After that, annual follow up.
Some practitioners continue to offer screening to women with good life expectancy > 65 that have risk factors (history of abnormal screening, current smoker or history of smoking, unknown screening history, previous HPV-related disease, new partners, immunocompromised, in utero diethylstilbestrol exposure). The timing to stop is unknown, but they often use 80 years as a cutpoint. This approach is questionable.
Below three useful algorithms, more can be seen at the ASCCP website:
BONE MASS DENSITY SCREENING GUIDELINES:
Who to screen?
All Women > 65 (USPSTF, AAFP)
Women <65 with a risk 10 year risk of fracture* => than a 65yo white woman with no additional factors. (USPSTF, AAFP)
Women <65 with a previous fracture or with significant risk factors (ACOG)
Men only if clinical manifestations of low bone mass, such as radiographic osteopenia, history of low trauma fractures, and loss of more than 1.5 inches in height, as well as in those with risk factors for fracture (UpToDate)
How to screen?
Dual-energy X-ray absorptiometry (DXA). It usually assesses the T-score (what is expected from someone with 30yo with same sex and ethnicity) of the femoral neck and lumbar spine.
How often to screen?
People being treated for osteoporosis – Every 1-2 years
Low bone mass (T-score -2.00 to -2.49) or with risk factors for ongoing bone loss = DXA every 2 years. (UpToDate)
Low bone mass (T-score -1.50 to -1.99) with no risk factors = DXA in 3-5 years. (UpToDate)
Normal or slightly low bone mass (T-score -1.01 to -1.49) = Follow up DXA in 10-15 years. (UpToDate)
Risk Factors: Previous fracture, glucocorticoid therapy, low body weight, current cigarette smoking, excessive alcohol consumption, rheumatoid arthritis, secondary osteoporosis (premature menopause, hypogonadism, liver disease, IBD)
* The 10 year risk of fracture can be calculated using the FRAX tool. The 10 years risk of fracture for a 65yo white woman with no additional factors is 9.3%
BREAST CANCER SCREENING GUIDELINES:
Breast cancer screening strategies diverge immensely between different societies. Below we summarize the most common approaches:
Who to screen?
Women aged 40 to 49 with average risk – Individualized discussion (discuss with the patient risks vs benefits).
Women aged 50 to 74 with average risk – Everyone should be screened, there is just discussion about how often (1 vs 2 years) and what methods (mammography alone vs mammography + clinical exam)
Women aged 75 or older with average risk – Patient may or may not be screened after this age. The screening may continue if the life expectancy is of at least 10 years (ACC) or at least 5-7 (ACR).
Women aged 25+ with high risk* – High risk (parent, sibling or child with breast cancer, BRCA1 or BRCA2 gene) may be screened earlier (no earlier than 25). Women with history of breast radiation between 10-30 years may start screening after 8-10 years with annual MRI and mammography (no earlier than 25) – ACOG also recommend clinical exam).
How often to screen:
Women aged 40 to 49 with average risk – Annual (ACOG, ACR, ACS) or Biennial (USPSTF, ACP)
Women aged 50 to 74 with average risk – Annual (ACOG, ACR, ACS*) or Biennial (USPSTF, ACP, AAFP, ACS*). * For ACS 50-54 should be annualy and 55-74 biennial.
Women aged 75 or older with average risk – Patient may continue screening if life expectancy is > 10 years (ACS) or if patient desires to after discussion (ACOG), at the same intervals mentioned above.
Women aged 25+ with high risk* – ACS = Annual Mammogram; ACOG = Every 6 months breast exam + Annual mammogram PLUS breast MRI PLUS breast self-exam; ACR = Annual mammogram PLUS MRI
What methods to use for screening?
Women aged 40 to 49 with average risk – Mammogram (USPSTF, ACS, ACR, ACP, AAFP) or Mammogram + Clinical exam (ACOG)
Women aged 50 to 74 with average risk – Mammogram (USPSTF, ACS, ACR, ACP, AAFP) or Mammogram + Clinical exam (ACOG)
Women aged 75 or older with average risk – Mammogram (USPSTF, ACS, ACR, ACP, AAFP) or Mammogram + Clinical exam (ACOG)
Women aged 25+ with high risk* – ACS and ACR = Annual Mammogram PLUS MRI; ACOG = Every 6 months breast exam + Annual mammogram PLUS breast MRI PLUS breast self-exam.
* High risk is characterized by personal history of ovarian, peritoneal, tubal, or breast cancer; a genetic predisposition (BRCA or other susceptibility genes); prior radiotherapy to the chest; or other breast cancer risk factors, such as a strong family history, resulting in a calculated lifetime risk of developing breast cancer of greater than 20 percent
Average risk is a lifetime risk of breast cancer <15%. This can be calculated with the Breast Cancer Risk Assessment Tool.
USPSTF = U.S. Preventive Services Task Force
ACOG = American College of Obstetricians and Gynecologists
ACR = American College of Radiology
ACP = American College of Physicians
ACS = American Cancer Society
AAFP = American Academy of Family Physicians
SOURCES & FURTHER READING:
- Cervical Cancer Screening Guidelines for Average-Risk Women – CDC
- Cervical Cancer: Screening – USPSTF
- ASCCP Algorithms for Cervical Cancer Screening/Results
- Breast Cancer Screening Guidelines for Women – CDC
- USPSTF Breast Cancer Screening. Originally published on: December 30, 2013.
- USPSTF Osteoporosis Screening